If you click “Continue” below, you will leave the current site and be taken to a site maintained by a third party that is solely responsible for its content. Amgen provides this link as a service to website visitors. Amgen is not responsible for the privacy policy of any third-party websites. We encourage you to read the privacy policy of every website you visit.*




Identifying each patient’s risk status helps you tailor your treatment
plan to
achieve their recommended level of LDL-C.10
2018 AHA/ACC/Multi-society guideline definition of
very high-risk ASCVD10


Low percent of patients receiving statins ± ezetimibe achieve
LDL-C < 55 mg/dL
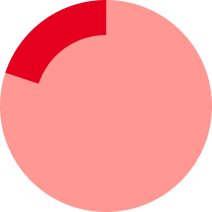
20%with low to
moderate
intensity statin

26% with high-intensity statin
Based on the 2022 ACC ECDP recommendation for patients with ASCVD at very high risk8
*After evaluating the optimization of lifestyle, adherence to guideline-recommended statin therapy, risk factor control, statin associated side effects, and escalating to high intensity statin if not already taken.
AHA/ACC = American Heart Association/American College of Cardiology; ASCVD = atherosclerotic cardiovascular disease; ECDP = Expert Consensus Decision Pathway; MI = myocardial infarction; PAD = peripheral artery disease.